What technology is needed for telehealth?

Let’s talk telehealth equipment. For some organizations, this can be the most daunting step in the process to implement your telehealth program. But the truth is, your setup can be quite simple.
There is no one-size-fits-all for telehealth programs. Your use cases will affect your technology requirements. By assessing what’s right for your providers, your patients and your budget, you can find a solution that works for you.
Let’s look at the most common equipment and how it’s used.
The basics.
All you really need for a basic telehealth program are a software program to connect providers to other providers and/or providers to patients, a secure internet connection and a computer with video capabilities.
Software Platform: A telehealth platform that will allow for secure, real-time communication is essential. Telehealth software designed specifically for healthcare goes beyond what Skype can do, by providing HIPAA security and a way to collect data from the consultation.
When choosing a platform, look for:
- Real-time video and image streaming.
- Secure video, messaging and store-and-forward capabilities.
- HIPAA and HITECH compliance, ensuring safety for your patients’ sensitive information.
- Adaptability to your organization’s needs.
- Cloud-based technology, so users can access the platform anywhere and don’t need to download software.
Internet Connection: You’ll need a secure, reliable internet connection with enough bandwidth to connect via video.
Device with Webcam and Microphone: Most current laptop come equipped with a webcam, so you likely already have the basic equipment you need. If not, an external webcam is inexpensive and can be attached to your existing laptop or office computer.
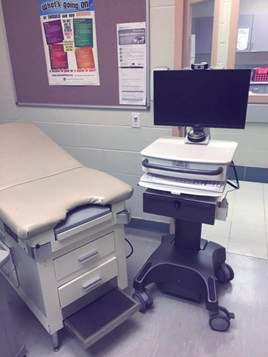
Mobile cart.
Here’s a Jackson and Coker telehealth mobile cart out on location helping physicians connect their patients with specialty care outside the practice. It can move from room to room, meaning the practice doesn’t have to dedicate telehealth space.
In a provider's home.
Integrated Computer: If your provider is working from home or another outside location, he or she will need a device that is able to connect to your telehealth platform with a secure internet connection and a webcam/microphone. With a cloud-based software platform, your providers can login from anywhere protected by the platform’s security.
In the exam room.
Diagnostic Tools: One day, it’s possible that all patients will have digital diagnostic tools in their homes. Some healthcare organizations are already using tools like home test kits, glucose readings and heart monitors.
Mobile Cart: A mobile cart holds your computer and diagnostic tools and can easily be moved from room-to-room, eliminating the need for investment in a dedicated telehealth space. Use one to connect your providers with specialists in other facilities, who can help diagnose or treat a patient from miles away.
Mobile Case: This is a compact system that you would only need if you conduct work in the field, such as disaster relief or homeless outreach.
At a patient's home.
Computer, Smartphone or Other Mobile Device: Seventy-seven percent of Americans now own a smartphone; and 95 percent of them own a cell phone of some kind. Your telehealth platform should be easy for a patient to access from a smartphone or computer, either through an app or browser.
Internet Connection: Patient access to a reliable internet connection is an ongoing hurdle towards full telehealth implementation. However, private companies and other lobbying groups are working to close broadband gaps, allowing for additional telehealth expansion. Also, most patients should be able to connect through their phone with data service.
A good way around this? Have patients access telehealth services by coming into your facility and using your dedicated computer or mobile cart.
Wearables: Devices including smartwatches and heart monitors will likely be an important part of future in-home healthcare. While they may not be necessary to start your program, depending on what services you’d like to offer, portable diagnostic tools and wearables for your patients may be an investment you’ll likely need to make in the coming years.
Ongoing needs.
Data Collection: Your program should have some way to collect data after a consult and save it for patient records. Providers can record patient information directly in the EMR while communicating through the telehealth platform, ensuring that data is consistent regardless of whether the appointment is in-person or online.
Provider Training: As you bring on additional providers to your telehealth program, who will teach them to use the platform? Consider the complexity of the platform you select for your facility. Jackson and Coker’s virtual care solutions require little or no training for the patient. Provider training typically takes less than 15 minutes.
IT Support: Who will provide support should technical problems occur in the future? Look for this in your contract with your software provider. Does the service extend beyond installation? If you have a larger organization, your current IT staff should be able to help. Make sure you have buy-in from those people and narrow your selection of telehealth platforms to those that require only hardware support from your IT staff. Many solutions offer 24/7 technical support for the software, which means your IT staff isn’t burdened with learning, installing and troubleshooting a new program.